Health Info
How to Treat Common Pediatric Problems
After reading this information, please feel free to discuss any questions you may have with your child’s pediatrician during your next office visit. This information looks to answer most of the basic questions that parents have, so be sure to read over this carefully before calling our office. If you still have concerns after reading this information, then please don’t hesitate to call us.
Fever
Call Us Immediately if your child is less than three months old and has a fever of 100.3°F (Unless he has received immunizations within 24 hours) or if the fever is over 105°F.
If your child looks or acts very sick be sure to call us immediately as well.
Description - If your child’s rectal temperature is over 100.3°F or if their oral, axillary (armpit) or tympanic (ear) temperature is over 100.0°F, they have a fever.
Should your child feel hot to the touch, we ask that you take their temperature by one of the above means prior to your calling us. The body's normal temperature when measured orally is 98.6°F, but it can fluctuate during the day. An increased temperature of up to 101° F can be caused by exercise, excessive clothing, a hot bath or hot weather. Warm food or drinks can also raise the oral temperature of your child. If you suspect such an environmental cause for increased temperature of your child, cool them down and take their temperature again in a half hour.
Causes and Expected Course – A fever is the body's normal response to getting an infection. Many times, these are viral illnesses, but a few can be bacterial illnesses. A fever helps fight infections by turning on the body's immune system. Normal fevers (100.3 to 104°F), which all children get, are not harmful. They usually last for two to three days and the temperature of the fever normally doesn't relate to the seriousness of the illness. How sick your child acts is what you should really be looking for. A fever causes no permanent harm until it reaches 106°F.
Studies have shown that nearly 4 % of children between the ages of six months to six years will have a brief convulsion due to a fever. Should your child have a convulsion due to a fever, we ask that you do not panic. If the convulsion lasts less than five minutes, call us and immediately bring your child to our office or the nearest emergency room. Should the seizure last longer than five minutes, you will need to call an ambulance. This kind of seizure is harmless most of the time, but your child should still be seen by their doctor to make sure there isn’t a more serious underlying issue.
Treatment – When your child has a fever it is important for them to drink as much fluids as possible. Things such as popsicles and drinks with ice can be beneficial. During a fever, important bodily fluids are lost due to sweating so it is important to counteract that. If your child is getting the chills or feels cold, be sure to only give them a light blanket. You may be tempted to bundle them up, but this will only lead to their fever increasing.
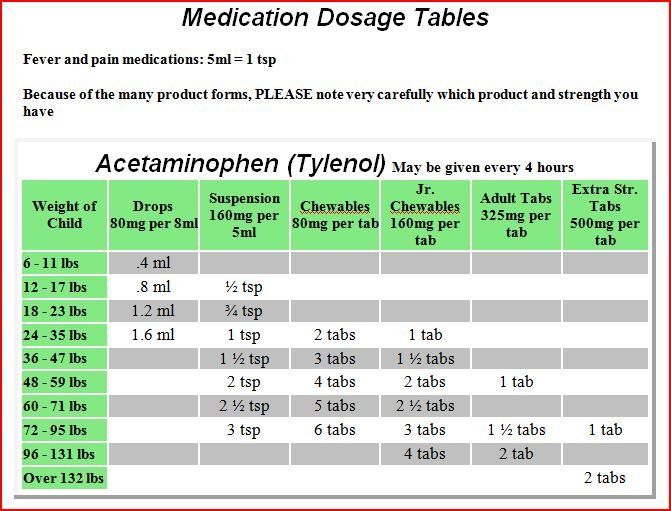
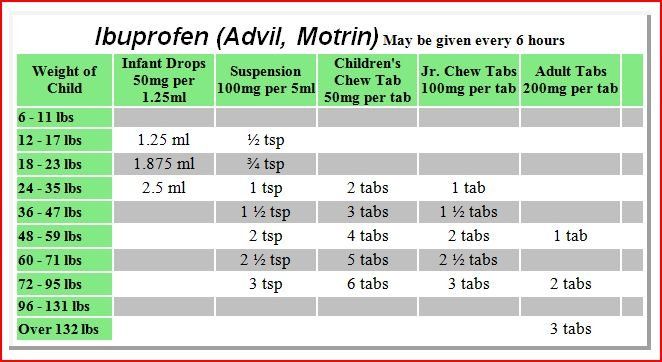
Other treatments to reduce a fever include sponging with lukewarm water, or slightly cooler water if the fever is nearing an emergency. It is also recommended to give them acetaminophen or ibuprofen before beginning the sponging. Sponging works much more efficiently than complete immersion, so it is suggested to sit your child in two inches of water while wetting the skin surface. Eventually cooling will begin with the evaporation of water. If your child should begin to shiver, raise the temperature or stop sponging until the acetaminophen or ibuprofen takes effect. No matter where the temperature was before this, it will most likely not dip below 101°F. Make sure that your child does not attend school for at least 24 hours after a documented fever.
It is important to remember that the fever is helping your child fight off their infection and that drugs should only be used if the fever is over 101°F. If your child is younger than 12 weeks of age and has a fever not associated with immunizations, call your doctor before giving them any acetaminophen or ibuprofen. If you are wondering if it is better to use acetaminophen or ibuprofen, one major advantage ibuprofen has over acetaminophen is that it is longer lasting (6-8 hours instead of 4-6 hours). If it has been suggested by your doctors to use both, you may want to use this method if the temperature is over 103°F and does not go down using only one medicine. If the high fever continues to last for more than 24 hours, call our office.
**We do not recommend aspirin or aspirin-containing products like Alka-Seltzer for any fever. Please read product labels.
Vomiting
Description - Vomiting is the emptying of a large portion of the stomach's contents through the mouth or nose. In contrast, spitting up is the bringing up of one or two mouthfuls of stomach contents. Spitting up is a naturally occurring issue in children under the age of one.
Cause and Expected Course – In most cases, vomiting occurs because of a viral infection of the stomach or when your child eats something that does not agree with them.
The vomiting will normally stop within six to 24 hours. Changes in the diet can usually lead to a speedy recovery. Often, a child experiencing vomiting caused by a virus may also experience diarrhea that can last for several days.
Treatment – Only give your child clear fluids up until eight hours have passed without vomiting. For infants, it is suggested to use an oral electrolyte solution such as Pedialyte or Kao Lectrolyte. For a child over one year of age, they can have flavored Pedialyte or Gatorade. For a child over two years, you may give them water, caffeine-free cola, lemon-lime soda or popsicles. It is important to stir the soda until most of the fizz is gone as the bubbles can inflate the stomach and increase the chances of continued vomiting. Start slowly with one teaspoon to one tablespoon of clear fluid and repeat every five to 10 minutes.
After two hours without vomiting, you can begin to increase the volume of clear fluids. If your child vomits using this treatment, rest the stomach for one hour and then start over but with smaller amounts. The one teaspoon at a time approach rarely fails. Once eight hours have passed without vomiting, your child can slowly return to a bland diet. Infants are suggested to start with foods such as cereals and bananas. If your baby
only uses formula, give one or two less ounces per feeding than normal. Older children can eat things such as saltine crackers, white bread, rice and mashed potatoes, along with soups like chicken and rice or noodles. In most cases, your child can be back on a normal diet within 24 hours. For breast-fed babies, we suggest providing breast milk in smaller amounts than usual. If your baby vomits once, make no changes. If your baby vomits twice, continue breast-feeding but nurse on only one side for 10 minutes every one to two hours. If your baby vomits three or more times, nurse for four to five minutes every 30 to 60 minutes. You can also give your baby an electrolyte solution between breastfeedings. Once eight hours has gone by without vomiting, return to normal nursing on both sides.
A common error is to give as much clear fluid as they ask for instead of slowly increasing their dosage. This will more often than not lead to continual vomiting. We ask that you also be aware that oral medicines can irritate the stomach and make vomiting much worse. If your child has a fever over 102°F however, you can administer acetaminophen. Call your physician if your child is vomiting and needs to continue taking a prescription medicine.
Call us immediately should your child shows any signs of dehydration such as no urine in over 8 hours, an extremely dry mouth, no tears when crying, etc. If your child vomits up blood or green liquid be sure to also contact us as soon as possible.
Call us during office hours if the vomiting continues for more than 24 hours if your child is under two years of age, or more than 48 hours if your child is older than two. Do not continue to give Pedialyte alone for over 24 hours without contacting us.
Diarrhea
Description -
Diarrhea is the increase in the frequency and water content of bowel movements. Mild diarrhea is the passage of a few loose bowel movements, while severe diarrhea is the passage of watery, sometimes green BMs. To better understand the severity of the diarrhea, you should be looking at the frequency of the episodes. The main concern with diarrhea is dehydration due to the loss of body fluids.
If your child is experiencing dry mouth or an infrequency of urination, they are most likely experiencing dehydration.
Cause and Expected Course -
Diarrhea is normally caused by a viral infection of the intestines. It can many times be caused by bacteria like Salmonella or parasites and occasionally can be induced by a food allergy or drinking too much sugary fruit juices. It can also be caused by antibiotics your child may be on. The diarrhea can last anywhere from a day to a week and will need to be monitored to make sure dehydration does not take place. Always make sure your child is taking in enough liquids.
Treatment – The best form of treatment is an increase in the amount of fluids that your child is ingesting. There are a few diets that are listed below that will also aid in getting rid of the diarrhea in as little time as possible.
Formula-Fed Infants (Less Than One Year Old) With Diarrhea -
If your baby
has mild diarrhea, continue a regular diet with a few minor tweaks. It is suggested that you continue with the usual strength formula but in smaller quantities than normal. You can also administer Pedialyte in between feedings. Should your baby be able to eat solid foods, you can give them things including rice, cereal, mashed potatoes, applesauce, strained bananas, and strained carrots. Avoid all fruit juices; they make diarrhea worse.
If your child has moderate to severe diarrhea as well as dark urine, give Pedialyte or Kao Lectrolyte. Should your child resist the taste of either it is suggested that you add a bit of Kool-Aid mix to help them take it better. Your child should drink as much of this as they want as the main goal is to prevent dehydration. It is important to never restrict fluids when your child has diarrhea. If your baby absolutely refuses to take Pedialyte, you may try Gatorade or decaffeinated cola, lemon-lime soda and/or sweetened decaffeinated tea. We do not suggest making a homemade electrolyte solution because an error can cause salt poisoning. After being given clear fluids for four to eight hours, your baby will be very hungry. It is suggested that you go back to the formula and offer it more frequently in the small doses than you had previously. If the diarrhea does not begin to slow down, then you should consider a soy or lactose-free formula. Often there is less diarrhea with these because of the absence of milk sugar (lactose). If you do choose soy or lactose free formula, then you should keep your baby on it for up to three days after the diarrhea has subsided.
Older Children (Over 1 Year Old) With Diarrhea – If the diarrhea is mild, it is more than alright to have them on a regular diet with a few changes. They should eat more foods containing starch that include cereal, breads, crackers, rice, noodles, mashed potatoes, bananas, broiled chicken and hard-boiled eggs. Yogurt can also be a good option during this time.
As stated above, it is important to drink more liquids, especially water. Avoid all fruit juices. Make sure that they are also drinking less fruit juice, avoiding milk and other dairy products (except for yogurt) and anything that may cause bowel movements, such as beans.
If the diarrhea is moderate to severe, make sure your child is getting enough flavored Pedialyte, water or a variety of Gatorade, sweetened decaffeinated tea and decaffeinated soda for the first 24 hours. If it continues for more than one day, offer milk as well with the above fluids.
Breast-Fed Infants with Diarrhea -Bowel movements of a breast-fed infant can be anything from watery to soft. Bowel movements like this are normal unless they contain mucus, blood or develop a bad odor. During the first two or three months of life, the breast-fed baby normally has one BM after each feeding. However, if your baby's BMs dramatically increase in number, your baby probably has diarrhea. You can also determine if they are experiencing issues if they aren’t eating normally, are acting sick or have a fever.
If the mother’s diet contains coffee, color herbal teas this may be a contributing factor to the loose BMs. If your breast-fed baby has diarrhea, treatment is straightforward. Continue to breast-feed but at more frequent intervals. When you stop breast feeding it can lead to greater problems. If the diarrhea worsens and becomes more frequent, give Pedialyte between breastfeedings for six to 24 hours. If your baby is taking solids, you may try small feedings of those foods listed above. You may have to stop breast feeding temporarily if your baby is too exhausted to nurse and needs intravenous fluids for severe diarrhea and dehydration. Pump your breasts to maintain milk flow until you can breast-feed again.
Other Aspects – Be sure to never use boiled skim milk. This is very dangerous and can cause major complications for babies with diarrhea as it contains a large amount of salt. More fluids than normal with a gradual return to a bland diet is usually the best medicine. Too little or too much fluids can lead to further issues. Remember, diarrhea is very contagious, and you should always wash your hands after changing diapers or using the toilet.
The skin around your baby's anus can become irritated by the diarrhea. Wash the area around the anus after each BM and be sure to put petroleum jelly around the area. Also, it is important to use diapers with snug leg bands or cover the diapers with a pair of plastic pants.
Vomiting with Diarrhea – Should your child vomit more than twice, follow the recommended treatment for vomiting instead of this treatment for diarrhea until your child has gone eight hours without vomiting.
Call us immediately if there are signs of dehydration that include no urine in more than 8 hours, a very dry mouth, no tears or if more than a few specks of blood appear in the diarrhea. If the diarrhea is severe (more than eight BMs in eight hours), if the diarrhea is very watery and your child also vomits the clear fluids three or more times, give us a call.
Call us during our office hours if mucus or pus appears in BMs, if a fever over 100.3°F lasts for more than three days or diarrhea lasts for more than a week.
Abdominal Pain
Cause and Expected Course – There are many causes of stomachaches, but stomach pains are often caused by something simple like overeating, drinking too much soda pop, or other types of indigestion. Sometimes a stomachache signals the onset of stomach flu with vomiting or diarrhea soon following.
The most common causes of abdominal pain are stress and worry. Over 10% of children have recurrent stomachaches from stress.
Causes of stress in children can include changing schools, moving, death or serious illness in the family, divorce and major world events. The pain occurs in the pit of the stomach or near the belly button. These stomachaches can have numerous causes and should be treated. In smaller cases, the pain is normally better or gone in two hours. In more serious causes, the pain worsens or becomes constant.
Treatment -
Your child should lie down and rest until they are feeling better. Generally, a warm washcloth or heating pad on the abdomen for 20 minutes can speed the recovery process. Do not give your child solid foods and make sure they only take sips of clear fluids. Younger children are likely to refer to nausea as "a stomachache”, encourage them to sit on the toilet and try to pass a BM. This may relieve pain if it is due to constipation or impending diarrhea. It is important to not give medications for stomach cramps unless you have spoken with your pediatrician and it is asked that you avoid laxatives, enemas and painkillers.
If your child has been evaluated by a physician and gets stomachaches from stress, try to help your child worry less. Children with recurrent stomachaches tend to be sensitive, serious, conscientious or even model children. It is suggested that you talk about the reasons they are feeling these pains and how they can better cope with them. Make sure that your child doesn't miss any school because of stomachaches. Children have a tendency to want to stay home when they are stressed. Teach your child to use relaxation exercises for mild pains; have them lie down in a quiet place, take deep, slow breaths and think about something pleasant.
Call us immediately if the pain is severe and lasts more than one hour, if the pain is constant and has lasted more than two hours, if the pain comes and goes and lasts for more than 24 hours or if the pain is in the scrotum or testicle or in the lower abdomen on the right side. Always call us if your child starts acting very sick.
Colds
Description -
A cold or upper respiratory infection is a viral infection of the nose and throat. Most often these symptoms can be a runny or stuffy nose, fever, sore throat and cough, and sometimes hoarseness, red eyes and swollen lymph nodes in the neck.
Colds are oftentimes confused with other issues, such as vasomotor rhinitis and chemical rhinitis. Vasomotor rhinitis involves patients having a runny nose in the wintertime when they are breathing cold air.
The nose usually stops running within 15 minutes after a person comes indoors. This is obviously not a cold and will not require any treatment. Chemical rhinitis involves a dry, stuffy nose cause by using nose drops that constrict blood vessels too often and/or for too long (longer than 1 week).
Cause and Expected Course – Colds can be spread from one person to another by hand touching, coughing and sneezing and are never caused by cold air or drafts. There are over 200 viruses that cause colds and most healthy children get at least six colds per year. If they get a fever with the cold, it should normally not last any longer than three days, while nose and throat symptoms last for about a week. It is important to lookout for signs of secondary bacterial infections such as earaches, yellow drainage from the eyes, sinus pressure or pain or difficulty breathing.
Babies, especially those under three months of age, with a persistent cough frequently have bronchiolitis or pneumonia. If you have a young infant, make sure that he or she does not get dehydrated and make sure to call your pediatrician if these problems persist.
Treatment – There is not much that can be done to change how long a cold will last. However, we can relieve many of the symptoms. Most stuffy noses are blocked by dry mucus. Using saline nose drops and then suctioning out or blowing the nose can be helpful. Make sure to use a clean eyedropper to put drops into the nose. For an infant who cannot blow his or her nose, place three to four drops of saline in each nostril before each feeding. Several times a day you may use a soft rubber suction bulb to gently remove the loosened mucus. If your child is breastfeeding or bottle feeding, you need to clear his or her nose, so he or she can breathe while feeding. It is also extremely important to clear your baby's nose before you put him or her down to sleep. For an older child who can blow his or her nose, use three to four drops in each nostril while your child is lying flat on a bed. Wait one minute for the water to soften and loosen the dried mucus then have your child blow his or her nose. This can be repeated several times for complete clearing of the nasal passages. We do not recommend using these medications in babies under nine months of age. Avoid using multi-symptom products, especially those that contain Tylenol, and be sure to use cold medication for nasal symptoms and use cough medicine for coughs. Even if your child has a fever, cold and cough, these multi symptom products normally do not have the ideal amount of medication for each symptom. We strongly recommend that you limit your choices to a few preparations and that you carefully follow the directions on the label. Do not give leftover antibiotics for uncomplicated colds because they have no effect on viruses and may be harmful.
Prevention of Colds -
A cold is caused by direct contact with someone who already has a cold. Hand washing is the most important method of limiting the spread of colds. Throughout the years, we are all exposed to colds and develop some immunity to them. Complications from colds are more common in children when they have yet to develop these immunities. Try to avoid undue exposure of young babies, especially those less than three months of age, to other children or adults with colds in places such as nurseries. Vitamin C, unfortunately, has not been shown to prevent or shorten colds. Large doses of vitamin C (for example, 2 grams) cause diarrhea.
Call us immediately if breathing becomes fast and heavy, if your baby under 3 months of age has a persistent cough, or if your child starts acting very sick.
Call us within 24 hours if the fever lasts more than three days, the runny nose lasts more than 10 days, the eyes develop a yellow discharge or the cough is getting worse. Call us if you can't unblock the nose enough for your infant to drink adequate fluids or if you think your child may have an earache or sinus pain. You must get a throat culture if your child's throat becomes sore.
Coughs
Description -
The cough reflex releases air and secretions from the lungs with a sudden force. The cough can be dry and hacking or wet and mucus producing. Serious coughing bouts can last up to five minutes.
Cause and Expected Course -
Most coughs are caused by a viral infection in the trachea/windpipe or bronchi, the larger air passages in the lungs. Most children get this viral infection a couple of times per year in addition to a cold.
You should remember that coughing is an important part of the recovery process as it clears the lungs and protects them from pneumonia. If your child has bronchitis, it will cause a dry cough that lasts two to three weeks. Sometimes the cough becomes loose and wet for a few days with your child coughing up a lot of mucus and can be a sign that the illness is nearly over.
Treatment – When treating a cough, it is important to have your child take in warm liquids to relax the airway and loosen up the mucus. Have them start with warm apple juice or warm herbal tea (unless your child is younger than four months old) and be sure to never add liquor. Cough-suppressant drugs do stop coughing; however, the cough reflex helps protect the lungs. Be sure to only give your child cough-suppressants if the cough is interfering with their sleep, school attendance or homework. If you do wish to give your child a suppressant, we recommend over-the-counter Robitussin DM or Delsym. Follow the directions on the package and remember that cough medicines will not make the cough go away any quicker. If there is dry air, it will tend to make coughs worse but putting a humidifier into the child’s room can help with this issue. It is highly advised to stop smoking while your child is going through this. If they enjoy drinking milk, they may still do so and if they are breast feeding they can continue with the same routine.
Call us immediately if breathing becomes fast or labored.
Call us during office hours if a fever over 100.3°F lasts for more than three days. If the cough lasts more than seven days or if you have other concerns or questions, feel free to give us a call.
Earaches
Description - Earaches are normally caused by bacterial infections of the middle ear or the space behind the eardrum. They are usually complications of a cold, with the congestion caused by the cold blocking off the eustachian tube (the passage connecting the middle ear to the back of the throat).
If the eustachian tube is blocked for too long, fluid builds up in the middle ear, which becomes infected.
Once the fluid builds up for long enough, it will create great pains for your child’s inner ear, which will begin to bulge.
Irritability, poor sleep and a fever are common with an earache. Most children have at least one ear infection a year with over a fourth of these children having more than one infection. The pressure in the middle ear may cause the eardrum to rupture and drain a yellow, cloudy or bloody fluid. This small hole will usually heal within a week.
Children are most susceptible to ear infections between the ages of six months and two years, but they can be a common occurrence up until the age of eight.
Treatment –
- Antibiotics - Give your child the antibiotic as prescribed. The medicine will kill any bacteria that are causing the ear infection. Make sure to not miss any doses because your child is sleeping. If a prescription states to take it every eight hours, and you know your child will be sleeping during that time, give the first dose of the day as soon as your child awakens and give the final dose just prior to them going to sleep. If the medicine is in liquid form, store the antibiotic in the refrigerator and use a measuring spoon to be sure that you are giving the exact amount. Give your child the medicine until the bottle is empty or the pills have all been taken. Make sure you do not save the antibiotic for the next illness because it will not be as effective over time. Even if your child feels better in a few days, give the antibiotic until it is completely gone or for the complete number of days prescribed your doctor.
- Pain Relief - Acetaminophen and ibuprofen can be used to aide with an earache or fever over 101°F for several days until the antibiotic takes effect. These medications can begin to control the pain within one to two hours. Eardrops can also be used to reduce the pain, especially at bedtime.
- Restrictions -
Your child is more than welcome to go outside and does not need to cover the ears. Swimming is permitted but no diving is suggested, as that can put extra pressure on the ears. Air travel is also safe when your child has an earache, but they need to make sure to swallow fluids, suck on a pacifier or chew gum during descent. Ear infections are not contagious, and your child can return to school when the pain reduces.
- Ear Recheck – It is suggested that your pediatrician see your child two to four weeks after they have gotten over the infection. They will be sure to make sure that is gone completely and will recommend a follow up appointment if your child is prone to these infections.
- Prevention of Ear Infections -
If your child gets regular ear infections it is important to protect them from second-hand tobacco smoke and reduce their exposure to colds during the first year of life. Try to delay the use of large day care centers and breast-feed your baby during the first six to 12 months of life.
Call us immediately if your child has a stiff neck or is more lethargic than usual when they are sick.
Call us within 24 hours if your child complains of a persistent ear pain, if the fever or pain is not gone after your child has taken the antibiotic for 48 hours or if you have other questions or concerns.
Sore Throat
Description – If your child gets a sore throat, it will be obvious with the complaining about the pain they are experiencing. Children that are too young to talk may have a sore throat if they will not eat or cry during feedings.
Cause and Expected Course – The majority of sore throats are caused by a virus and are part of a cold. Nearly 10% of sore throats are caused by the streptococcal "strep" bacteria. The way to find out what is causing the sore throat is with a throat culture or rapid strep test.
Children who sleep with their mouths open may wake up in the morning with a dry mouth and sore throat. It feels better within an hour of having something to drink then you should have a humidifier placed in their room during the night. Sore throats caused by viral illnesses normally last three to four days. Strep throat can be eased with penicillin and other antibiotics. Once a child has taken the strep medication for 24 hours, they are no longer contagious.
Treatment –
- Local Pain Relief -
Children that are older than one are encouraged to sip warm chicken broth or apple juice. You can also give your child popsicles and soft foods if they prefer. Give your child acetaminophen or ibuprofen for the sore throat or for a fever over 101 degrees Fahrenheit.
- Common Mistakes in Treating Sore Throat–Make sure to not use expensive throat sprays or throat lozenges. They are no more effective than a hard candy and can contain an ingredient, benzocaine, that can cause an allergic reaction. Do not use leftover antibiotics from siblings or friends; those should be thrown out when used as they will not be as effective over time. It is also important to remember that antibiotics only help sore throats that are caused by strep and have no effect on viruses.
Call us immediately if your child is drooling or having great difficulty swallowing, your child is having difficulty breathing or your child is acting very sick.
Call us during office hours to schedule an appointment for a throat culture if your child has had a sore throat for more than 24 hours. The throat culture is not urgent; however, it is important to treat strep throat within seven days.